On the record with Sinai CEO Karen Teitelbaum

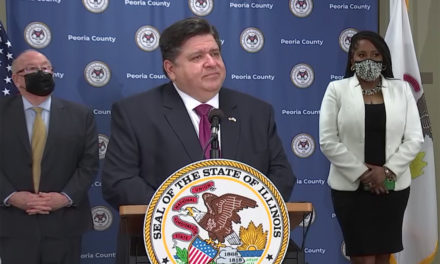
Sinai Health System CEO Karen Teitelbaum is among eight health system CEOs who have been meeting regularly with the Chicago and Illinois public health departments as the COVID-19 crisis unfolds.
The initial discussions focused on building capacity for a potential surge of patients, and included ethical decisions on what would happen if ventilators ran out.
Now, as the numbers have flattened, Sinai and other systems are reopening their doors to some of the elective procedures that were halted to make space for COVID-19 patients.
During a Health News Illinois webinar this week, Teitelbaum discussed the financial toll of the crisis and the likelihood of another resurgence.
She also highlighted the disproportionate impact that the pandemic is having on the minority communities her system serves.
Read more below.
HNI: How long do you think it’s going to be before hospitals like Sinai are fully open and patients feel fully ready to go back to a hospital setting?
KT: I think that we’re not going to see what was our normal for a very, very long time. I think that’s true of hospitals and, of course, I think just virtually everything else in our lives. In Sinai and the communities that we serve, there’s a tremendous burden of comorbidities. So hypertension, diabetes, congestive heart failure, and we also know that 96 percent of mortalities in the COVID situation have a comorbidity. So our communities do tend to be more in need of care than you might find in other select communities. So our patients are probably going to be coming back because the needs are going to be more pronounced than you might see, for example, in Streeterville, the Gold Coast or Lake Forest.
HNI: Has Sinai had any issues with acquiring enough personal protective equipment?
KT: I am really happy to say that throughout this whole crisis, the enormous civic generosity and the generosity of the philanthropic foundations throughout the city have been just outstanding. We’ve received many, many donations of masks, face shields and gloves. Our goal was to have at least 10 days worth of inventory because then we could put in another order and we would always make sure that we have enough inventory. So even though we made the decision early on for the protection of our caregivers – and we’ve got about 3,200 caregivers, so it’s not a small organization – and for the protection of our patients, we have not had an issue with that. Right now we’ve got about 10 days of just about everything, so we are feeling very, very comfortable.
HNI: How likely is it that there will be another resurgence?
KT: I used to feel very confident about saying I think that we’re through the worst. But I don’t think I would say that anymore. I think just walking around in my own neighborhood in River North and seeing how many people are walking around without face masks, even though it’s an executive order, I believe. I just hope that people will take the social distancing seriously. This is not going to be, you know, we flip a switch and tomorrow we can go back to normal. My fear is that many people are so ready for normal and so long for it, that we’re going to go way too far to the other side.
HNI: What’s been the financial impact of COVID-19 on Sinai?
KT: There are two things. One is that we as a hospital community lost revenue. Sinai lost 90 percent of our outpatient revenues when we stopped the electives. It was the right thing to do, of course, we’re going to do it. But that presented an immediate challenge. The second challenge is that COVID patients are in such intense acuity that the staffing that we have for those patients, instead of say, four patients to one nurse or five patients to one nurse, you have more of intensive care level staffing, which would be one-to-one or two patients to one nurse. We try to keep it to that. And it depends on how acute the patients are. We prepare for that. The other thing is there’s more equipment, there’s more medication, there’s more protective equipment. So the cost to treat a COVID patient is much higher than a typical patient. So it’s like a double whammy for the health system. Sinai estimated that we are losing, for every month that this continued, $10 million per month.
HNI: How are you making up for that?
KT: A couple of things. One is philanthropy. Again, the Chicago community has stepped up. There’s a COVID community fund that’s been a wonderful plus. There’s a number of funders who have stepped up and have helped not only Sinai but the entire hospital community. So that was one piece, but that does not cover even a month’s worth of loss for us. But from the federal dollars, we’ve all read about the CARES Act that was the federal stimulus dollars to help hospitals. And there were three buckets of money that have been distributed so far. In the first one, Sinai got a little bit more than $5 million, in the second one we got a little bit more than $5 million. It sounds like a lot of money, but when you think about what I told you we lose every month, it’s only just helping us to stay afloat. In this last tranche of money, we received a much bigger piece, as many hospitals did, and it was based on the number of COVID patients you’re treating. And we have I think (as of Wednesday), we’ve got between our two acute care hospitals about 85 patients in house, or who are being tested. But those dollars are not supposed to be a windfall. They’re not supposed to be a profit, it doesn’t help invest in anything here. Those dollars simply try to cover the cost from COVID. We know, again, it’s not flipping a switch. The volumes are not going to come back right away. So it’s going to be a gradual process.
HNI: What changes have you made in response to COVID-19 that could last after the crisis?
KT: We at Sinai have rethought how can we deliver care. For example, we amped up our telehealth services. We had telehealth for psychiatry, which is huge. But now we’ve expanded that and we’re finding it works for a number of people. It works as well as an office visit for some. And for some, it’s even more convenient for a number of reasons. So I think we’re going to retain and maybe invest more in telehealth. Our workforce… I’m kind of lonely in this suite, because we’ve sent home all of what’s called our nonessential workers. If you’re not on the front lines, you were sent home. Our leaders are here to be visible to the front line, and to help the front-line folks. But what that taught me was that we really can do more of a remote workforce and that will enable us to close some of our older buildings if we’re emptying that out. So there are a lot of things we hadn’t thought about.
HNI: COVID-19 has exposed the health inequities present in many parts of Chicago, and across the country. How has this impacted the patients you serve?
KT: COVID has really laid bare the racism that Sinai has known all along because of the communities that we treat. Our patient base is pretty much on the west and southwest sides of Chicago, half African American, half Latinx. And, as I said before, a tremendous burden of comorbidities for a number of reasons. And since the people hardest hit by COVID are those with comorbidities, we’re seeing that now. So when we know that the Latinx population accounts for 26 percent of all the deaths that we’re seeing in the city, and the African American population accounts for, as of this week, I think it was 48 percent. Whites account for 19 percent. You see where that big difference is coming in. Across the city and the state, the mortality rate is about 4 percent. At Sinai, our mortality rate is about 15 percent because so many of the people we serve have these comorbidities. And addressing these disparities is something that Sinai has been doing for 100 years. So when all of a sudden it seems like it’s a big revelation, I’m sitting there thinking, ‘Well, what have we been telling you?’ Obviously people know, but this has really shone a spotlight on it because it’s everything that comes with poverty. Many of our community members don’t have homes in which they can socially distance the way that some of us can. There’s a density. Many of our community members have to take public transportation and depend on their jobs. There are single female heads of households who have to have their jobs. So it’s just a very different situation. We serve a number of undocumented people in the community, and they are coming in only when they’re gravely ill because they’re afraid to come and get healthcare. So you see how this whole picture of poverty, unemployment, comorbidities, it all comes together to paint a picture that’s a lot more challenging in terms of COVID.
HNI: What role do you think health systems going forward need to play in addressing these health inequities?
KT: One thing that we’ve known is we can’t do it ourselves. That’s not how it works. Everything that we do, we partner with community organizations. It’s not the health system coming in and saying, ‘I’m going to tell you what you need.’ Everything is driven by our community partners, whether it’s federally qualified health centers or partners that are doing work on workforce development, which is tied to keeping people healthy, and housing, which is tied to keeping people healthy. We all have to be working together. The communities have what’s called quality of life plans, which looks at all the things that keep a community healthy and vibrant. In addition to your healthcare services, it’s education, it’s employment, it’s housing. And we have to be part of that. And we have to make sure that all of those parts are working together. People returning from the justice system. We’ve got to get people enrolled in healthcare, and we need to get them jobs. One of my goals is to hire as much as possible from our communities.
HNI: There appears to be mounting frustration among safety nets and some other hospitals with the state’s Medicaid managed care program. What do you think is driving this growing frustration with Medicaid and does Sinai share in any of that frustration?
KT: I don’t know that it’s a growing frustration. When the state moved to manage Medicaid, and with the right intention…there were a lot of growing pains, no question, I think on both sides. Everybody had a kind of new system to get used to. And not only did you have one payer. I think the first year we had 12 payers. Now we’re down to five or six. So that was a big difference. So you think about that shift, all of a sudden you’ve got 12 different ways of doing things. So that was frustrating. Are there still issues that need to be addressed? Yes. And the Legislature I think has been a good friend to the healthcare community. Look, everybody’s first priority is, ‘Let’s make sure that the people of Illinois who are enrolled in Medicaid are getting high-quality care and they’re getting the right care when they need it.’ And that the providers are getting paid the right amount and in the right amount of time. That’s what we all should be focusing on. I do want to give a shout out to the Illinois Health and Hospital Association. In full disclosure, I’m a board member, but even if I weren’t, I would say that the Illinois Health and Hospital Association has really worked hard to make this a good environment for three partners: the state, the insurance companies and the providers. For Sinai, over the last two years we’ve worked individually. I had CEO to CEO meetings with each of our payer partners to talk through, ‘Here are the challenges that we’ve got, what can we do to mitigate that?’ And most of the time, the CEOs had no idea. And we were able to work together to resolve issues that were troubling to us. We have what’s called joint operating committees between our staff, our case management staff, or clinicians and the managed care organizations. And we found it’s not perfect yet, no question. But Sinai always tries to be more collaborative in the process. And in this case, I think it has served us well. So we try to work things out together feeling that we all have the best interest of the patients in mind.
Health News Illinois is removing the password on all stories related to the coronavirus. For the latest developments follow us on Twitter at @healthnewsil or check out our website. For complete healthcare coverage, sign up for a free trial to our daily email newsletter.