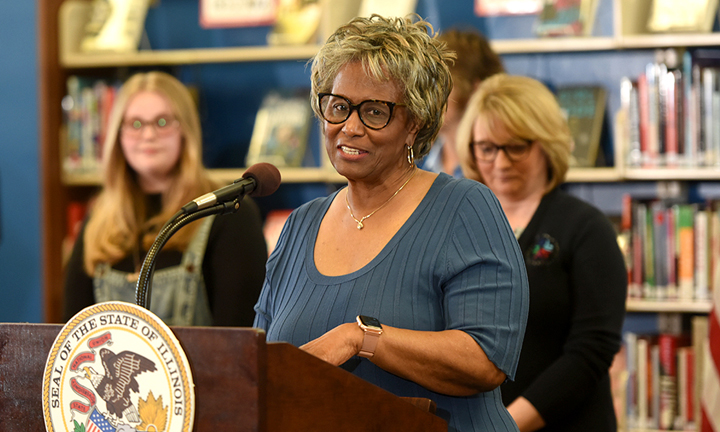
Sen. Doris Turner, D-Springfield, wants state regulators to go after Blue Cross Blue Shield of Illinois over network adequacy and what she calls “inadequate” 2023 health plans.
Her letter to Department of Insurance Director Dana Popish Severinghaus comes a year after Blue Cross announced that Springfield Clinic would no longer be in network. Officials say the move impacted about 55,000 members across central Illinois.
IDOI announced this spring it fined Blue Cross Blue Shield of Illinois’ parent company, Health Care Service Corporation, $339,000 for failing to submit requested information following the termination of its contract with Springfield Clinic.
Turner said in her letter that she still hears concerns from constituents about network adequacy.
“Any consumer that elects a BCBSIL insurance plan will have been misled by their online physician directory and insistence that their network of providers is adequate under the law,” Turner said.
A spokeswoman for IDOI said they appreciated the letter and that a network adequacy filing for Blue Cross is under review.
“We take seriously our regulatory authority of health issuers offering plans on and off the ACA health insurance marketplace, and if a provider network is found to be inadequate, the department will take the appropriate steps,” she said.
Blue Cross said in a statement that its proposed plans meet network adequacy requirements as set by state law, and that they offer a “robust network” in the Springfield region with more than 3,000 in-network providers.
“Blue Cross and Blue Shield of Illinois is committed to providing our members affordable and accessible coverage across the state,” they said.
Chase Hammon, chief financial officer for Springfield Clinic, said they continue to work to find a compromise with Blue Cross. He added they are “not optimistic” about an agreement.
“We are disappointed that our efforts to restore access to thousands of patients that need an adequate network of physicians in our communities have not been more fruitful,” he said.