Rush CEO Dr. Omar Lateef on the impact of the omicron-fueled COVID-19 surge on Chicago

After the worst COVID-19 spike of the entire pandemic, Rush University Medical Center CEO Dr. Omar Lateef said this week they are starting to see positive signs that the region is past the peak of the omicron-fueled surge.
“Our numbers are starting to decline,” he told Health News Illinois. “We are getting less admission through our emergency room. We’re getting less people call with symptoms, and we’re getting less requests for tests. So when you look at that trend, each one of them is in a different level of severity, but all of them are seemingly going down.”
Lateef also spoke of how the region’s providers came together to support one another during the recent winter surge, how the healthcare workforce is holding up and what the healthcare industry can learn from the pandemic.
Edited excerpts are below.
HNI: Where are things as of (Wednesday) at Rush and the region as it relates to the omicron-fueled surge?
OL: The initial pandemic from two years ago was sort of a shock and awe presentation. To answer your question, you really have to sort of take a step back and understand what the limitations are during a pandemic. And there are really three issues that come up. Do you have enough supplies to care for patients? Do you have enough beds? And do you have staff?
For the first couple waves, or what we later called surges, of the pandemic, we didn’t have enough supplies. And that’s what you heard across the country, sort of the supply chain crisis. How do we get masks? How do we get IV tubing? How do we get things like that? The second issue was beds. The concern was we were going to run out of beds, and if you recall, New York City and Chicago commandeered large arenas and filled them with beds. We always seemed to have had staff, staffing was never one of the issues.
So when you ask, ‘How are we faring during the current surge?’, I would say that we learned a lot from the first several surges and that we have adequate supplies in this country. We are well stocked for supplies to take care of COVID patients, and we have an ample enough number of beds. Our issue today, and our issue this surge, was related to staffing. We didn’t have enough staff beds to ramp up for a potential increased need. And here’s the good news, we seem to have stayed just below, in Chicago, overcoming our ability to supply staff beds for people. I think in conjunction with other hospitals, we’ve all been able to bend, but nobody broke and we didn’t have patients overflowing from our community. But where we are now is we’re starting to see the numbers start to decline, and that’s a really optimistic sign for the future.
HNI: Chicago Department of Public Health Commissioner Dr. Allison Arwady said Wednesday afternoon that Chicago has passed the peak of the current surge, do you see that to be the case as well?
OL: It’s exactly what we’re seeing. I think the city has done a pretty amazing job of being transparent about where the numbers are. And that’s sometimes bad news and sometimes good news. And today the good news is really reflected in what we’re seeing on the ground and in the front line. Our numbers are starting to decline. We are getting less admission through our emergency room. We’re getting less people call with symptoms, and we’re getting less requests for tests. So when you look at that trend, each one of them is in a different level of severity, but all of them are seemingly going down.
HNI: How is the Rush workforce holding up during this current surge?
OL: So the good news at Rush is the workforce is extremely dedicated and managed to compensate for those who are out sick. There’s been a perfect storm on the workforce. Since 2013, we predicted a shortage in staffing in healthcare in this country. It was multifactorial. There were more people retiring. There’s an aging population of healthcare providers, less people coming into the field and a dramatically growing population. So when you put all of that together, you’re going to have an outsized need for staffing than you had for providers. The pandemic accelerated that and put a spotlight on that. Omicron accelerated it even more because our staff themselves got sick. It was so infectious at any point in time, we had as many as 3 percent to 5 percent of our staff on furlough. And so when your front line is sick, other people had to give up whatever free time they had to do extra work. And the beauty of what we saw not just at Rush, and we absolutely saw it at Rush, but we saw it all through healthcare in America, where people were stepping up and doing extra shift after extra shift. An incredible amount of both dedication and persistence on the part of our front-line staff. That’s an American identity and it was amazing to watch and you really saw that during omicron.
HNI: How have the region’s health systems and providers worked together during this surge to help one another?
OL: In many ways, that pandemic highlighted some of the country’s healthcare flaws. We all live a little bit in isolation. We’re competing healthcare systems all throughout this country, even though we may be geographically close to each other. What the pandemic allowed us to do is put … that competitiveness aside and just load-balance resources across the community to better care for the community. And we highlighted that during the surges in our effort to take the patients that we felt we can make a difference for from wherever they were in the community. Many other healthcare systems did that, and you saw that partnership develop. We also saw the city of Chicago, as well as the state, do a pretty amazing job of coordinating efforts to make sure no one area was overburdened. And so by providing the right information, providing resources and providing a constant stream of crowdsourcing all the hospital leaders throughout all the surges of the pandemic, we’ve been better able to share resources when others needed it.
HNI: Given how many more people are getting COVID during this wave, do you expect an uptick in long COVID cases? If so, what is Rush doing to prepare for that?
OL: I’ll answer the second part first. Rush set up a long-haulers clinic. We’ve set up services to track people, to follow people, both to study them from an epidemiological perspective to make sure we can help add to the science, but to make sure more importantly that we can provide care for people with ongoing symptoms. So we’ve opened up access, we’ve dedicated people to taking care of patients that are suffering from prolonged symptoms.
In truth, anybody that tells you they know what’s going to happen long-haul for omicron has tremendous Nostradamus-like skills. How we learn in science is by studying what happens and going back and saying, ‘OK, this percentage of people within the ages of 5 through 10, they develop these symptoms and they lasted this long.’ We follow this cohort for this long, and this cohort for this long. And we really look at that evidence, and that evidence retrospectively allows us to draw conclusions, and then we use those conclusions to predict the future. What’s been so difficult about this pandemic was we didn’t have the luxury, since it was a new infection, of knowing what would happen. So we do our best guesses in science. So what we know about any virus is there is a subpopulation of people that can develop prolonged symptoms for a variety of reasons. Many of those reasons are because they had an underlying condition, and they were just weakened and that underlying condition got worse, or it may be related to the virus itself. I think the honest answer to the question of what will be the long-term effects of omicron is that time will tell. It’s not a way of skirting the question, but rather an honest approach to say that without the data right now, it’s almost impossible to predict.
HNI: What, if anything, do you see as the long-term effect on healthcare from the surge we’ve seen this winter in Chicago and nationwide?
OL: I think the pandemic, not just omicron, but the entire pandemic, is a call for action for us in healthcare to figure out better ways to share resources across healthcare. It’s a call to action about recognizing that access, while we’ve known for a long time is a critical problem in this country, it was highlighted during the pandemic. And if we recover from this pandemic and don’t change access across this country, then we haven’t taken advantage of our learnings from this pandemic. So I think the pandemic represents a call to action to improve healthcare so that everybody in this country has equal access to getting good outcomes.
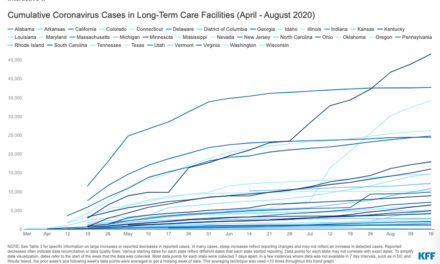
HNI: We’ve heard some hospitals have had issues with discharges to long-term care facilities during the most recent surge. What has been Rush’s experience there?
OL: The same way hospitals had a staffing crisis, so did the step-down facilities that we transfer patients to. And so what happened was, when we had this sort of what I would call the labor crisis in healthcare, and as people got sick, the number of staff beds in the facilities we would transfer a patient to were less. Last year was a longer period of time it took to get a patient transfer. Everybody was working hard, there just weren’t the same number of people able to work because people were literally on furlough, they were literally unable to leave their house for five days. And because of that, our length of stay did increase. We’re starting to see that already self-correct. We’ve also seen both the state and the city try to put measures in to make it easier to discharge patients.
HNI: What are the plans for Rush in 2022? Are there any major priorities or growth strategies that may have been delayed because of the pandemic?
OL: Here’s what we learned in the pandemic. We learned that being all-in and just being a COVID hospital isn’t the best thing that we can do for our community, that people’s conditions continued regardless of the pandemic or not. So if you had heart failure pre-pandemic, you had heart failure post-pandemic. So during even this last surge, we maintained our ability to care, invest and grow our strategic programs because we are a pillar in our community and we recognize that importance. And so what I would say is for the future, we’ve doubled down on our commitment to our community, and we’ve doubled down on our commitment to provide improved access and to enhance our key strategic programs. So we’re going to grow in cancer, we’re going to grow in neurosciences, we’re going to grow across the board because we realize that our community has continuing healthcare needs. The pandemic, while it delayed that, certainly didn’t stop it. So our plan is to reinvest even more in our core values.