Illinois congressional members encourage insurers to provide more financial relief

Democratic members of Illinois’ congressional delegation have called on the state’s insurers to provide immediate financial relief to individuals, families and small businesses.
In a letter sent this week to the heads of seven insurance organizations, the lawmakers requested each insurer issue maximum premium credits to enrollees of their plans, guarantee access to COVID-19 diagnostic testing and treatment with no forms of cost sharing, and provide other forms of assistance to the fullest extent possible.
“We encourage you to now also step up and share the massive profits you are experiencing from reduced healthcare utilization during COVID-19 with your enrollees throughout our state,” the letter said.
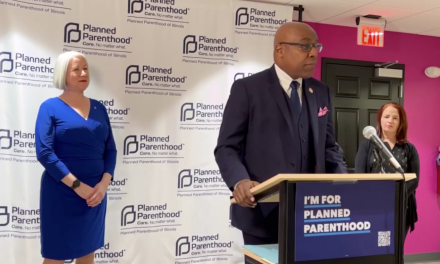
Lawmakers who signed onto the letter include U.S. Sen. Dick Durbin and Reps. Jan Schakowsky, D-Evanston; Lauren Underwood, D-Schaumburg; Robin Kelly, D-Matteson; Jesús G. “Chuy” García, D-Chicago; Danny Davis, D-Chicago; and Cheri Bustos, D-Moline.
In response, insurers said they have taken a variety of steps to aid members, front-line workers, partners and other patients during the pandemic.
UnitedHealth Group said in a statement it has waived cost-sharing for COVID-19 testing and treatment, provided members $1.5 billion in premium and other relief, accelerated $2 billion in payments to providers and invested more than $100 million in community-based philanthropic efforts.
“We remain committed to correcting any imbalances that may continue in the months to come, and to providing additional rebates to customers and members as appropriate,” the statement said.
A spokesman for Health Care Service Corporation said in a statement they will respond to the lawmakers’ letter, but added they are waiving cost sharing for COVID-19 testing and treatment, expanding access to care including telehealth services with no additional costs, extending approvals on medical and behavioral health services, and partnering with community organizations to provide direct relief to those who need it the most.
“Throughout the pandemic we have taken numerous actions to support our customers and members, just as we always have,” he said.
Humana said in a statement it immediately waived COVID-19 cost sharing requirements for Medicare Advantage and other members. It also waived all out-of-pocket medical costs for primary care, behavioral health care and telehealth visits for its Medicare Advantage members; as well as created a dedicated, clinically-focused, outbound system that connects with members one-on-one to help meet their needs.
“Humana is committed to supporting our members, providers, and the communities we serve during these unprecedented times,” the company said. “Our focus has been on addressing needs in real-time, and we fully expect that the impact we have experienced from deferred care will be offset by the direct support we’re providing to help these groups, as well as by higher claims costs in the second half of this year.”