Safety net hospitals call on state to renegotiate Medicaid managed care contracts

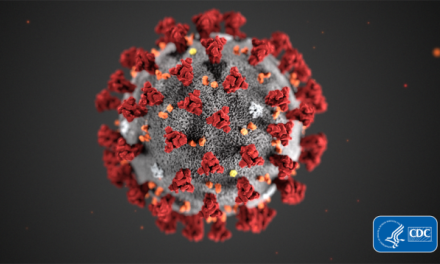
A coalition of safety net hospitals is calling on the state to renegotiate Medicaid managed care contracts as they watch their revenues plummet from the COVID-19 crisis.
Hospitals across the state halted elective procedures in March to conserve resources for COVID-19 patients. But the safety nets argue that because they are disproportionately reliant on Medicaid funds, they can’t absorb the losses in the same manner as general acute care hospitals, “who have sizeable reserves and the ability to cross-subsidize losses with commercial payers.”
Meanwhile, they say, managed care organizations are still being paid capitated rates reflective of pre-COVID-19 volume trends that are not being realized.
“Rather than allow the MCOs to keep those profits, we ask that the funds instead be redirected to the safety-net hospitals that are on the front lines, serving the communities and people most affected,” wrote the CEOs of Norwegian American Hospital, Loretto Hospital, St. Bernard Hospital, Roseland Community Hospital, South Shore Hospital, Swedish Covenant Hospital, Jackson Park Hospital and Medical Center, Mercy Hospital and Medical Center, Thorek Memorial Hospital and Methodist Hospital.
The letter comes as the state is facing increasing pressure from hospitals over Medicaid managed care. Another safety net, Saint Anthony Hospital, sued the state last week over Medicaid payments. And Mercyhealth recently announced it’s canceling its MCO contracts with the state.
Department of Healthcare and Family Services spokesman John Hoffman said the department has been working to “rapidly direct resources to Medicaid members and providers especially in low-income communities of color where the pandemic is hitting the hardest.”
“Hospitals have begun receiving added stability payments from HFS throughout the state in the fight against COVID-19, and the department is arranging for more support through the managed care program,” he said.
The safety nets, in their letter, say the enhanced rates for COVID-19 are not covering their costs.
Norwegian American Hospital CEO Jose Sanchez said revenues at his hospital are down 50 percent, and they are facing increased costs to retain workers and acquire personal protective equipment.
“The programs that have been the bread and butter of this hospital have been non-existent because we are primarily focused on addressing the needs of those patients who have chronic conditions or who have COVID in our hospitals,” he told Health News Illinois. “Our business has totally collapsed.”
Samantha Olds Frey, CEO of the Illinois Association of Medicaid Health Plans, said she doesn’t know anyone who thinks that COVID-19 will end up decreasing healthcare costs, especially in the Medicaid program. But if it turns out that plans are not spending enough of their money on healthcare services, that will show up in their medical loss ratios.
“If plans are overpaid, which we do not anticipate, they would have to return funding back to the state,” she said. “And then the state would use that as they see fit. I would imagine that would be to support the entire Medicaid program. However we do not anticipate that will be our reality.”
Sanchez said that for some hospitals that might be too late.
“We have a financial disaster on our hands right now,” he said. “I believe that post-COVID, many of these institutions may not even be able to survive, unless there is an infusion of cash.”
Health News Illinois is removing the password on all stories related to the coronavirus. For the latest developments follow us on Twitter at @healthnewsil or check out our website. For complete healthcare coverage, sign up for a free trial to our daily email newsletter.