Future of micro-hospitals in Illinois could hinge on lawsuit

As patient care increasingly shifts to outpatient settings, hospitals across the country are shrinking and some are rethinking their delivery models.
What that transformation looks like in the Land of Lincoln could depend in part on what happens with a lawsuit over a proposed 13-bed facility northwest of Chicago.
Late last month, a state appellate court heard arguments on whether Mercyhealth should be allowed to construct a so-called micro-hospital in Crystal Lake.
Similar-sized facilities have gained steam in other states. And in 2017, the Health Facilities and Services Review Board signed off on MercyHealth’s project. But Advocate Health Care and Centegra Health System argued the board did not follow its statute when approving the hospital.
A circuit judge sided last year with Advocate and Centegra and overturned the state’s approval.
At issue is the review board’s statute that says any hospital located within any of the state’s major metropolitan areas must have a minimum of 100 medical surgical beds. Crystal Lake is considered part of Chicago’s Metropolitan Statistical Area.
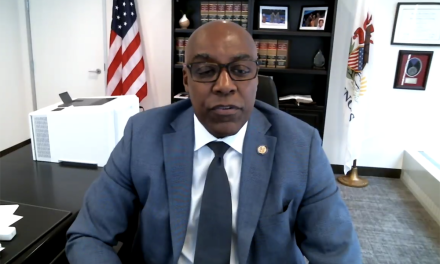
Assistant Attorney General Richard Huszagh, representing the review board, told the appellate court that the board has discretion when it considers applications. Though the project did not meet the statutory requirement, Huszagh said the board weighed it against factors such as a need for service in the area.
“If they had insisted on that need being met by a 100-bed hospital, they would have massively increased the overcapacity and that is one of the factors that this statute is intended to avoid,” he said. “The board is charged by the statute with balancing the unmet needs and avoiding overcapacity or underutilization.”
In this particular case, Timothy Eaton, an attorney representing Mercyhealth, argued the beds at the proposed facility would be transferred beds from an existing, underutilized facility in the county. The step was intended to have the “least impact” on other area hospitals, he said.
Attorney Hal Morris, representing Advocate, argued that the 100-bed minimum was a rule the board has not changed, despite previous opportunities to do so. That, he said, is proof it is more than just a suggestion that the board can choose to ignore.
“By not changing it, that is evidence that it is the rule,” Morris said during the appellate court hearing.
Anu Singh, managing director at Kaufman Hall, said the trend of micro-hospitals varies by market. They typically appear in regions where a health system sees a need for health services, but not enough to justify a traditional hospital with a range of services.
The smaller facilities have additional benefits, Singh said. Along with more personalized care, he said the size can be less overwhelming for patients.
“I think this is one of those situations that our industry, as we transform, that we may see some costs, scale and resource benefits of the micro-hospitals,” Singh said. “But we might also at times stumble upon a better solution from the patient’s eyes as well.”
Jordan Shields, managing director at Juniper Advisory, said technology, advancements in drugs, migration trends and changes to reimbursement are factors in the shift away from traditional brick-and-mortar facilities.
That shift has been slower in Illinois due to its certificate of need program, which can prevent some forms of experimentation happening in other states, he said.
Shields is also keeping his eye on the more than $260 million set aside for transformation through the hospital assessment program. He said that could provide some guidelines about what sort of facilities may be allowed in the future.
“Care has changed and the infrastructure that we have in the state of Illinois is built for the way healthcare was delivered,” he said.
Health News Illinois is a nonpartisan, independent news service covering the Illinois healthcare beat. Sign up for a free trial to the newsletter here.